Pain is a universal experience, yet its management remains one of the most challenging aspects of healthcare. Chronic pain affects millions of people worldwide, leading to a significant reduction in quality of life, productivity, and overall well-being. Traditional pain management strategies often rely on opioids and non-steroidal anti-inflammatory drugs (NSAIDs), which can come with severe side effects and the potential for addiction. In recent years, there has been a growing interest in the role of the endocannabinoid system (ECS) and cannabinoids in pain management, offering new hope for those suffering from various types of pain.
This article will explore the intricate relationship between the endocannabinoid system and pain perception, delve into the different types of pain, and examine the therapeutic applications of cannabinoids in alleviating discomfort. We will also discuss current research findings on the efficacy of cannabinoids in pain management and consider the future of this promising field.
Understanding the Endocannabinoid System
To appreciate the role of endocannabinoids in pain management, it is essential to understand the ECS itself. The ECS is a complex cell-signaling system that plays a crucial role in maintaining homeostasis within the body. It consists of three main components:
- Endocannabinoids: These are naturally occurring compounds produced by the body that bind to cannabinoid receptors. The two primary endocannabinoids are anandamide (AEA) and 2-arachidonoylglycerol (2-AG).
- Cannabinoid Receptors: These are found throughout the body and are primarily classified into two types: CB1 and CB2. CB1 receptors are predominantly located in the brain and central nervous system, while CB2 receptors are primarily found in the peripheral nervous system and immune cells.
- Metabolic Enzymes: These enzymes are responsible for the synthesis and degradation of endocannabinoids. They ensure that endocannabinoids are produced and broken down in response to the body’s needs.
The ECS is involved in various physiological processes, including mood regulation, appetite, immune response, and pain perception. When the body experiences pain, the ECS is activated, and endocannabinoids are released to help modulate the pain response.
The Mechanisms of Pain Perception
Pain is a complex phenomenon that can be classified into several categories, including acute pain, chronic pain, nociceptive pain, neuropathic pain, and inflammatory pain. Understanding these types of pain and their underlying mechanisms is crucial for effective management.
Acute Pain
Acute pain is a direct response to an injury or harmful stimulus, serving as a protective mechanism to prevent further damage. It is typically short-lived and resolves once the underlying issue is treated. Acute pain activates nociceptors, specialized sensory neurons that transmit pain signals to the brain.
Chronic Pain
Chronic pain, on the other hand, persists beyond the expected period of healing, often lasting for months or even years. It can arise from various conditions, including arthritis, fibromyalgia, and back pain. Chronic pain is often associated with changes in the nervous system, leading to heightened sensitivity to pain (central sensitization) and altered pain processing.
Nociceptive Pain
Nociceptive pain results from damage to body tissues and is typically characterized by a sharp, aching, or throbbing sensation. It can be further divided into somatic pain (originating from skin, muscles, and joints) and visceral pain (arising from internal organs).
Neuropathic Pain
Neuropathic pain occurs due to damage or dysfunction in the nervous system itself, often resulting in sensations such as burning, tingling, or shooting pain. Conditions like diabetic neuropathy and postherpetic neuralgia are examples of neuropathic pain.
Inflammatory Pain
Inflammatory pain is the result of tissue inflammation, which can occur due to injury, infection, or autoimmune diseases. This type of pain is often accompanied by redness, swelling, and heat in the affected area.
The Endocannabinoid System and Pain Modulation
The ECS plays a vital role in modulating pain perception through various mechanisms. When endocannabinoids bind to cannabinoid receptors, they can inhibit the release of pro-inflammatory cytokines and neurotransmitters, thereby reducing pain signaling. Here are some ways the ECS influences pain modulation:
- Inhibition of Nociceptive Pathways: Activation of CB1 receptors in the central nervous system can inhibit the transmission of pain signals from the periphery to the brain. This can help alleviate both acute and chronic pain.
- Reduction of Inflammation: CB2 receptors, primarily located in the immune system, play a crucial role in regulating inflammatory responses. When activated, they can help reduce inflammation, which is often a contributing factor to pain.
- Neuroprotection: Endocannabinoids have neuroprotective properties, which can be beneficial in conditions associated with neuropathic pain. They may help protect neurons from damage and promote healing.
Cannabinoids and Their Therapeutic Applications
Cannabinoids, the active compounds found in cannabis, can mimic the effects of endocannabinoids. The two most well-known cannabinoids are tetrahydrocannabinol (THC) and cannabidiol (CBD). While THC is primarily responsible for the psychoactive effects of cannabis, CBD is non-psychoactive and has gained attention for its potential therapeutic benefits.
THC and Pain Management
THC has been shown to have analgesic properties and is often used in the management of various types of pain, particularly chronic pain. Research has indicated that THC can:
- Reduce pain intensity: Studies have shown that THC can significantly reduce pain intensity in patients suffering from conditions such as multiple sclerosis, cancer, and neuropathic pain.
- Improve sleep quality: Chronic pain often disrupts sleep, leading to a vicious cycle of pain and insomnia. THC has been found to improve sleep quality, which can, in turn, help with pain management.
- Enhance the effects of opioids: Some research suggests that THC may enhance the analgesic effects of opioids, allowing for lower doses and potentially reducing the risk of opioid dependence.
CBD and Pain Management
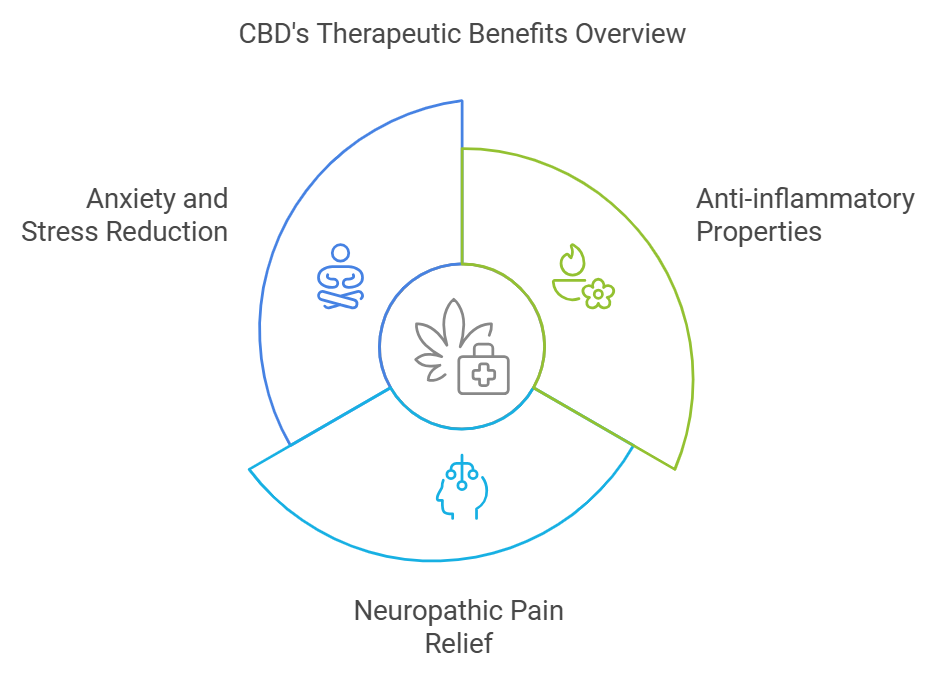
CBD has garnered significant interest due to its non-psychoactive nature and potential therapeutic benefits. Unlike THC, CBD does not bind directly to cannabinoid receptors but modulates the ECS and interacts with various other receptors, including serotonin and vanilloid receptors. Research on CBD’s efficacy in pain management has shown promising results:
- Anti-inflammatory properties: CBD has been shown to reduce inflammation, making it a potential treatment for inflammatory pain conditions such as arthritis.
- Neuropathic pain relief: Studies have suggested that CBD may be effective in alleviating neuropathic pain, providing relief for conditions like diabetic neuropathy and post-traumatic stress disorder (PTSD).
- Anxiety and stress reduction: Chronic pain is often associated with anxiety and stress, which can exacerbate the pain experience. CBD has been found to reduce anxiety and improve mood, potentially leading to better pain management outcomes.
Combination Therapies
The combination of THC and CBD, often referred to as the "entourage effect," is another area of interest in pain management. Some studies suggest that using a combination of cannabinoids may enhance their therapeutic effects while minimizing side effects. This approach allows for a more balanced and effective pain management strategy.
Research Findings on Cannabinoids in Pain Management
Numerous studies have explored the efficacy of cannabinoids in pain management, providing valuable insights into their potential benefits. Here are some key findings:
- Chronic Pain Studies: A systematic review published in the Journal of Pain found that cannabinoids were effective in reducing chronic pain, with many patients reporting significant improvements in pain levels and quality of life. The review highlighted the need for further research to determine optimal dosing and long-term effects.
- Neuropathic Pain: A meta-analysis published in the Journal of Neurology, Neurosurgery & Psychiatry concluded that cannabinoids are effective in treating neuropathic pain, particularly in patients with multiple sclerosis and HIV. The authors noted that cannabinoids could be a valuable alternative to traditional pain medications.
- Cancer Pain: Research published in the Journal of Pain and Symptom Management indicated that cannabinoids could effectively alleviate cancer-related pain, particularly in patients who do not respond well to conventional analgesics. The study highlighted the importance of individualized treatment plans, considering patient preferences and tolerability.
- Arthritis and Inflammatory Pain: A study in the European Journal of Pain found that topical application of CBD reduced joint inflammation and pain in animal models of arthritis. While more human studies are needed, these findings suggest that CBD may be a promising option for managing inflammatory pain conditions.
- Opioid Reduction: A growing body of evidence suggests that cannabinoids may help reduce opioid use in patients with chronic pain. A study published in the Journal of Pain found that patients using medical cannabis reported a significant decrease in opioid consumption, highlighting the potential for cannabinoids to serve as an adjunct or alternative to opioids.
Challenges and Considerations
While the potential of cannabinoids in pain management is promising, there are several challenges and considerations that must be addressed:
- Legal and Regulatory Issues: The legal status of cannabis varies widely across regions, impacting research opportunities and access for patients. In many places, cannabis remains classified as a Schedule I substance, which can hinder clinical studies and patient access.
- Dosing and Standardization: One of the significant challenges in using cannabinoids for pain management is the lack of standardized dosing guidelines. The effects of cannabinoids can vary widely based on individual factors such as metabolism, tolerance, and the specific condition being treated. This variability makes it difficult to establish clear dosing recommendations. More research is needed to determine optimal dosages and delivery methods for different types of pain.
- Side Effects and Interactions: While cannabinoids are generally well-tolerated, they can cause side effects, including dizziness, dry mouth, changes in appetite, and cognitive impairment, particularly with THC. Additionally, cannabinoids can interact with other medications, which can complicate treatment plans. Patients should consult healthcare providers before starting cannabinoid therapy, especially if they are taking other medications.
- Lack of Large-Scale Clinical Trials: While there is a growing body of research on cannabinoids and pain management, many studies have small sample sizes or lack rigorous design. Large-scale, well-controlled clinical trials are needed to establish the efficacy and safety of cannabinoids for various types of pain comprehensively.
- Patient Education and Stigma: There is still a significant stigma surrounding cannabis use, which can affect patients' willingness to explore cannabinoid therapies. Education about the potential benefits and risks of cannabinoids is essential to empower patients to make informed decisions about their pain management options.
Future Directions in Cannabinoid Research
As interest in the therapeutic potential of cannabinoids continues to grow, several future directions for research and clinical practice can be identified:
- Personalized Medicine: The future of pain management may lie in personalized approaches that consider individual patient characteristics, including genetics, lifestyle, and specific pain conditions. Research into pharmacogenomics may help identify which patients are most likely to benefit from cannabinoid therapies.
- Exploring Other Cannabinoids: While THC and CBD are the most studied cannabinoids, other compounds found in cannabis, such as cannabigerol (CBG) and cannabinol (CBN), may also have therapeutic potential. Research into these lesser-known cannabinoids could lead to new pain management options.
- Investigating Delivery Methods: Different delivery methods for cannabinoids (e.g., inhalation, oral, topical, sublingual) may have varying effects on efficacy and onset of action. Research into the most effective delivery methods for pain management could enhance treatment outcomes.
- Long-Term Studies: More long-term studies are needed to assess the safety and efficacy of cannabinoids in chronic pain management. Understanding how long-term use affects pain perception, quality of life, and potential side effects will be critical in establishing guidelines for cannabinoid therapy.
- Integration into Pain Management Protocols: As evidence supporting the use of cannabinoids grows, there may be opportunities to integrate them into existing pain management protocols. Multidisciplinary approaches that combine cannabinoids with physical therapy, counseling, and other modalities may provide comprehensive pain relief.
Conclusion
The endocannabinoid system plays a crucial role in modulating pain perception, and cannabinoids offer a promising avenue for pain management, particularly for those suffering from chronic pain conditions. With their ability to interact with the ECS and influence pain pathways, cannabinoids like THC and CBD have shown potential in reducing pain intensity, improving quality of life, and serving as alternatives to traditional pain medications.
While challenges remain, including legal barriers, dosing standardization, and the need for more extensive research, the future of cannabinoid therapy in pain management looks promising. As our understanding of the ECS and cannabinoids continues to evolve, patients may have access to safer and more effective pain relief options that enhance their quality of life.
As we continue to explore the therapeutic potential of cannabinoids, it is essential to approach this field with an open mind, rigorous scientific inquiry, and a commitment to patient-centered care. By doing so, we can unlock new possibilities for pain management and improve the lives of millions affected by chronic pain.